I’ve experienced living on both sides of this diagram. For many years, before I finally got a celiac diagnosis, I thought I had non-celiac gluten sensitivity (NCGS) (sometimes referred to as gluten intolerance). I remember countless times being in restaurants, requesting a gluten-free menu, and the waiter asking “is this an allergy? or celiac?”, me replying “no” because I didn’t know any better at that time, and the waiter breathing a sigh of relief.
But honestly this reaction always felt pretty dismissive, because I felt like my needs would not be heard or taken seriously with the words “gluten-sensitivity” even though the aftermath of getting glutened would be very serious.
Gluten-sensitive folks do have varying degrees of tolerance for gluten cross-contact, but if someone is making their needs known, it doesn’t matter what they’re condition is called, they deserve to be heard. Let it be known that whether you have celiac or NCGS, gluten exposure is no joke, and you are worth being respected.
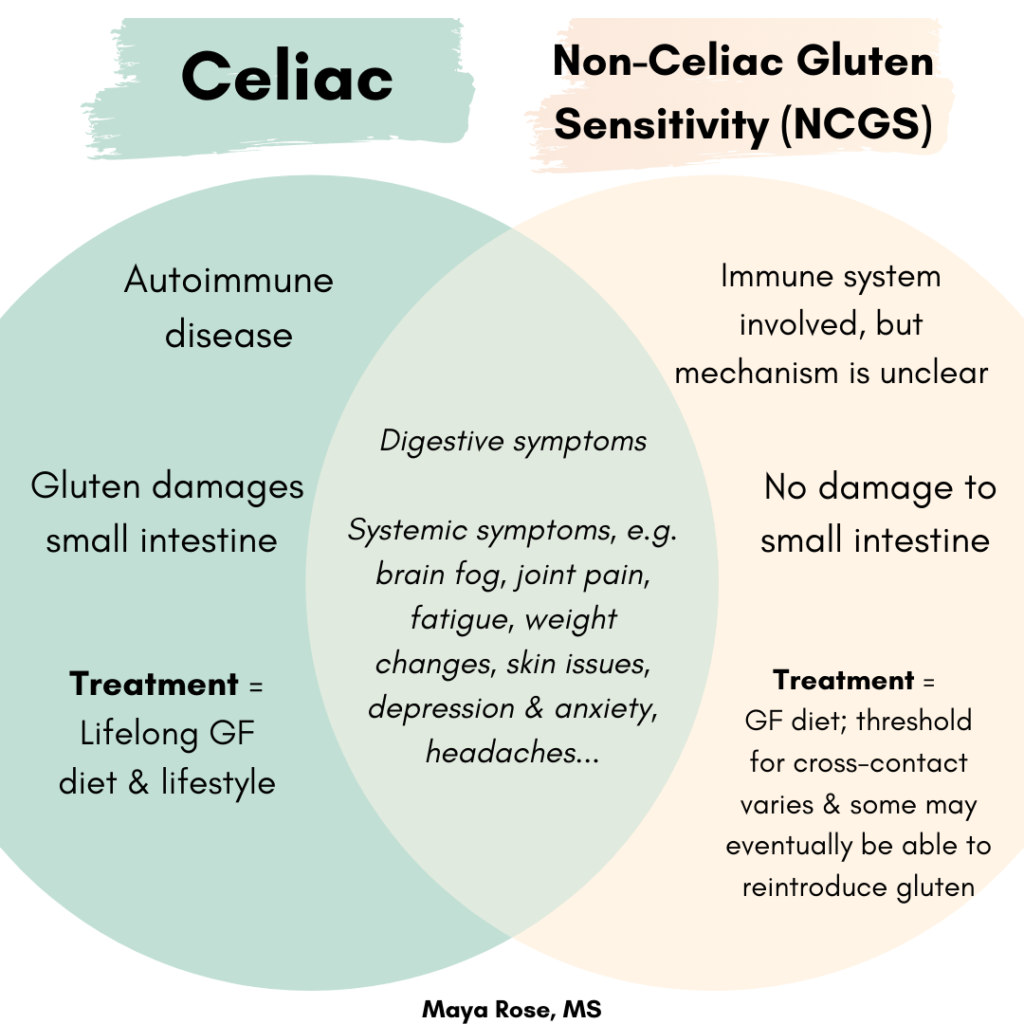
How do celiac and NCGS differ?
Although there is some wiggle room for cross-contact among NCGS folks (depending on the individual), there is no such thing for celiacs. Celiacs always have to take stringent precautions about avoiding gluten cross-contact based on the level of long-term risk that continued (even trace) gluten exposure presents.
Celiacs are affected by exquisitely tiny amounts of gluten, whether they show symptoms or not. That’s because even a teeny amount can trigger the autoimmune process and damage to the intestinal villi in celiac.
NCGS has been shown to activate the immune system to go rogue, but the exact way it does so is still being researched. What is known is that NCGS is a food sensitivity, not an autoimmune response (meaning your body does not attack itself). and does not damage the small intestine.
The damage to the small intestine that occurs in celiac leads to nutrient malabsorption and increased risk for certain conditions such as anemia, infertility, and osteoporosis. NCGS does not damage the small intestine in this way.
Treatment
Finally, the only treatment we know of at this point for celiac is a lifelong gluten-free diet and lifestyle. Those with NCGS have to do the same, although a very small few may find their tolerance changes over time (one more reason it’s so important to know if you have NCGS or celiac!).
How are celiac and NCGS similar?
For starters, they share the same trigger: gluten!
While the mechanisms, etiology, and nature of the two conditions are quite different, both are highly inflammatory, and they have MANY of the same symptoms in common. These include but are not limited to:
- Diarrhea, constipation, bloating, gas, abdominal pain, and/or nausea
- Headaches and migraines
- Brain fog
- Joint & muscle pain
- Fatigue
- Anxiety and/or depression
- Skin issues
- Numbness in the extremities
Note that the severity of these symptoms do not indicate one condition over the other. There are even many celiacs who are completely asymptomatic.
Get tested for celiac BEFORE you put the bread down
It’s important to find out whether you’re working with celiac or NCGS to know if the root cause of your symptoms are from an autoimmune disease or food sensitivity. If you have celiac, there are also different long-term risks and implications related to heredity, your chances of developing other conditions (especially autoimmune ones), and damage to the small intestine from gluten exposure.
Often when people start having gut issues, they are told by a practitioner to try cutting out gluten without first getting tested for celiac! This is honestly a huge and common mistake on the practitioner’s part, because it’s more difficult to test after someone has eliminated gluten. Typically, to get an accurate test result for celiac, you’d have to be eating 2-3 servings of a gluten-containing food for 6-8 weeks before. NCGS is diagnosed AFTER celiac is ruled out through an elimination/reintroduction challenge.
Personally, getting a definitive diagnosis of celiac was a GAMECHANGER for me. I wasn’t looking out for gluten cross-contact much before, because I didn’t know how vigilant I needed to be or that things like a gluten-free menu were not celiac-safe. Consequently, I was being exposed to small amounts of gluten on a regular basis, especially leading up to my diagnosis. I wasn’t living truly gluten-free, and my health and gut issues were very reflective of that. Becoming mindful about my need to prevent cross-contact made a HUGE difference for my health, which is one of the reasons I’m so passionate about helping my clients do the same.
That all being said, if you cut out gluten without being tested for celiac and do not want to do a gluten challenge due to the symptoms you’d experience, that is a completely understandable personal choice. However, in that case, you may want to consider mitigating cross-contact to the same degree as someone with celiac.
If you have questions, feel free to reach out!
